There are days when the skin seems tired too. It no longer responds to a favorite cream, looks dim and indifferent, stripped of its usual glow. It may feel like “just winter” or lack of sleep, but in fact this is the language of a body exhausted by emotions. When we learn to hear it, we notice: fatigue leaves a trace not only in the mind, but also on the skin.
Emotions that haven’t settled yet
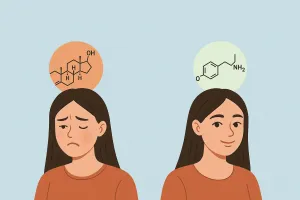
Our brain doesn’t distinguish whether the storm happened outside or inside. Any strong arousal is a potential threat, so it releases cortisol and adrenaline. The heart beats faster, vessels constrict, cutaneous microcirculation slows. It’s an evolutionary response: the body prepares to “fight or flee.” But in modern life there is nowhere to run, and unused energy remains as tension, microinflammation, and reactive skin.
Elevated cortisol alters the immune coordination of the epidermis; the barrier becomes more permeable, transepidermal water loss (TEWL) rises. Tightness, flaking, and itching appear, while creams that worked flawlessly a week ago suddenly seem ineffective. This is not a vague impression—it’s physiology, documented in clinical observation. A study in JAMA Dermatology showed that acute psychological stress slows the recovery of the skin’s barrier function, whereas reducing anxiety can facilitate its normalization. When the nervous system receives the signal “danger is over,” keratinocyte proliferation and barrier repair accelerate.
In short, each upheaval is a chemical event. Cortisol reshapes cytokine profiles, dampens lipid synthesis, and disrupts Langerhans cell function—the first line of cutaneous immune defense. After emotionally intense periods, we may see not only “paleness and dryness,” but reactive breakouts, itch, or localized inflammation.
How the skin “speaks” about fatigue
Sometimes the sign is subtle: a paler morning face than usual. Sometimes it’s obvious: flushed patches, small breakouts, the sense that no cream “sits” like before. Hypersensitivity isn’t a whim; it’s a consequence of sympathetic nervous system dominance. While the brain stays on guard, microcirculation is suppressed, regeneration slows, and facial muscles hold tension. In the mirror this reads as a mixture of weariness and vulnerability.
Dermatology even has a term for it—stress-related dullness. The skin loses tone, elasticity, and natural luminosity due to reduced perfusion and oxygenation. Dullness, flaking, and reactivity are not merely skin symptoms; the body is speaking for us. It asks for slowness, warmth, touch. Sometimes not a new product—but permission to exhale.

Silence and skin
Modern skin lives in noise—news, screens, notifications. For the nervous system this rivals cold or sleep debt. When the brain is constantly processing stimuli, it can’t enter repair mode, and hormones swing like a pendulum. On such days, skin “dims.” Relief comes not only from a cream, but from a ritual of silence. Five to ten quiet minutes before bed, and vessels receive a clear signal: it’s safe to soften.
The chemistry of calm
Some things restore us without words: warmth, breath, water, touch. Anything that lowers cortisol often lowers skin reactivity. A warm inhalation, a sip of water, a slow palm over the cheeks—these are micro-signals of safety. They prompt an oxytocin response—the bonding hormone that steadies the heart’s rhythm and lends suppleness to the skin.
“Oxytocin is linked to well-being and anti-stress effects.”
Frontiers in Neuroendocrinology
Scientists note: gentle, pleasant touch isn’t only an emotion. It activates the parasympathetic branch, supports oxytocin release, and tempers adrenaline spikes. That’s why massage, warm water, a blanket, or a tender self-touch can act as biological “switches” out of stress. For a deeper read on sensory regulation and the power of touch, see our piece How Much Touch Does the Body Need—how warmth and tenderness literally rewrite nervous system signals.
Light, rhythms, and the skin
Circadian rhythms govern not only sleep and mood but the skin’s barrier behavior. By day, defenses against oxidative stress dominate; at night, regeneration and collagen synthesis rise. When the cycle is disrupted (sunlight deficit, light pollution, late screens), the skin “lives” off-time—hypersensitive, dry, slow to heal.
A review in Nature Reviews Molecular Cell Biology confirms that the skin has an intrinsic clock coordinating repair and stress responses. Even brief natural-light exposure—an early walk, a moment by the window—helps resynchronize these processes and improve epidermal balance.
Scientific highlights
1) Psychological stress and the barrier. As shown in JAMA Dermatology, even short-term stress slows the closure of microdefects in the epidermis; reducing anxiety improved barrier recovery. It’s a direct demonstration of neural involvement in cutaneous regeneration.
2) Oxytocin and touch. The review in Frontiers in Neuroendocrinology links affective touch with oxytocin-mediated anti-stress effects and lower cortisol, explaining why simple rituals—hugs, warm showers, slow massage—have tangible therapeutic impact.
3) Circadian rhythms. According to Nature Reviews Molecular Cell Biology, the skin’s clock genes shape DNA repair, barrier renewal, and UV sensitivity. When rhythms are out of tune, reparative capacity falls.
Restorative rituals
Try slowing everything down—not only movements, but the logic of care itself. Evening: warm water, unhurried tempo. A soft towel, a few drops of oil in place of harsh toners. Let your hands move slowly—this is already therapy. Morning: open the window, let daylight rest on your face, do a brief palm massage. Daytime: spare a few minutes simply to feel your body—grounding, breath, shoulders melting down.
Give this a week and the barrier begins to “remember” its tasks: TEWL falls, reactivity fades. Not because you added another active, but because you removed excess threat signals. For a broader neurochemical context, revisit Mood Molecules: How Stress and Dopamine Affect Your Skin.
Care that soothes
A tired skin needs less stimulation and more support.
• Cleansing — minimal, non-stripping, no aggressive surfactants.
• Moisturizing — glycerin, hyaluronate, ceramides, squalane; a light occlusive layer at night.
• Anti-inflammatory vector — niacinamide, panthenol, β-glucan.
• Actives — only after the barrier stabilizes.
• Water temperature — moderate; extremes are vascular micro-stress.
Environment
Skin doesn’t exist apart from the air we live in. In winter, indoor humidity often drops below 40%, and even the best cream struggles if the air is dry. Add a humid point—a small humidifier or even a cup of water by the bed. Give your body 20–30 minutes of daylight, and keep gentle daily movement—these reduce systemic microinflammation and improve tone. Movement is the simplest way to activate lymphatic flow and restore a healthy hue.
A seven-day plan
- Days 1–2: remove irritants; switch to gentle cleansing; add richer emollients.
- Days 3–4: more light and warmth; breathing pauses; relax facial muscles.
- Days 5–7: re-establish calm rituals; assess reactivity—has tightness eased, has a soft glow returned?
When to see a specialist
If reactivity persists beyond two weeks, with itch or perioral flares, see a dermatologist. Even then, the foundation of recovery isn’t only formulation, but rhythm: the body heals no faster than we allow it to slow down.
Conclusion
Emotional fatigue has no scent or color, but the skin detects it first. It answers with silence, dryness, and loss of light—and through it, calm can return. When care comes not from duty but from tenderness, the barrier strengthens, muscles release, and the brain finally lets go. Beauty stops being a mask and becomes a state—a state where body and mind breathe in one rhythm.